M.D., F.A.C.S.
M.D., F.A.C.S.
Dr. Williams dedicates his practice to breast care. His clinical expertise is in both malignant and benign diseases of the breast. He focuses on comprehensive, minimally invasive and compassionate care of women and men with breast disease. He practices breast cancer surgery in Northern Virginia with offices in Haymarket, Brambleton and Chantilly, Virginia. He is a national leader in breast cancer education and founded the not-for-profit Breast Cancer School for Patients.
In 2019, he received a presidential appointment to be chairman of the President’s Cancer Panel at the National Instiute of Health. This panel is designated to serve as advisors to the President of the United States on the National Cancer Program.
Dr. Williams was the first Breast Surgeon in the state of Virginia to obtain from the American Society of Breast Surgeons simultaneous “Certification in Breast Ultrasound” and “Certification in Stereotactic Breast Procedures”.
In 2008, Dr. Williams founded the Novant – UVA Multidisciplinary Breast Cancer Conference in Haymarket, Virginia to enhance the “Team Approach” of breast specialists working together to treat this disease. This comprehensive approach has been embraced by our regional hospitals, medical community and most importantly, the community as a whole. In 2009, the UVA Community Health Breast Center – Haymarket, Virginia developed from this broad collaboration and Dr. Williams’ leadership. He served as medical director from 2009 to 2018 and resumed leadership in 2021.
Download Dr. Williams complete CV
(here)
Duke University (1984–88)
Durham, North Carolina
Bachelor of Science with Distinction in Psychology
University of North Carolina School of Medicine
Chapel Hill, North Carolina (1988 – 1992)
Doctorate of Medicine
Baylor College of Medicine (1992–1997)
Houston, Texas
Michael E DeBakey Department of Surgery
Internship & Resident in Surgery
Chief Resident in Surgery
Clinical Instructor in Surgery
1992-1997
American Society of Breast Surgeons
American Society of Clinical Oncology
American College of Surgeons, Fellow
American Board of Surgery, Certified
Michael E. DeBakey International Surgical Society
UVA Community Health Breast Center
INOVA Loudoun Hospital
INOVA Fair Oaks Hospital
UVA Health Haymarket Hosptial
UVA Prince William Hospital
Prince William Surgical Center
Haymarket Surgery Center
The Fauquier Hospital – Warrenton, Virginia
In Memory of Dr. Michael E. Debakey
1908 – 2008
Dr. Williams and his father, L. Polk Williams, Jr, MD, FACS both trained to become surgeons under the guidance of Dr. DeBakey at Baylor College of Medicine in Houston, Texas. Dr. DeBakey’s influence on Dr. Williams started at an early age through stories about him from his father. Dr Debakey was in the twilight of his surgical career when Dr. Williams trained with him, but his impact will be lifelong. Dr. DeBakey’s life motto was “The pursuit of excellence has been my objective in life.”
Dr. DeBakey is considered by many to be the greatest surgeon of the 20th century. He was an innovator of many cardiovascular surgical techniques and was a world-wide statesman for improving healthcare. He helped create the first M*A*S*H* units used in the Korean War, the Veterans Administration Hospital System, and led the creation of the National Library of Medicine. He held counsel with every U.S. President since Dwight Eisenhower. In 2008, at the age of 99, Dr. DeBakey was presented the Congressional Gold Medal by President George W. Bush. The Congressional Gold Medal is the highest civilian award given by the United States Congress in recognition of service to one’s country and humanity. Dr. DeBakey died on July 11, 2008.

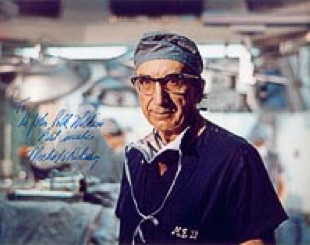
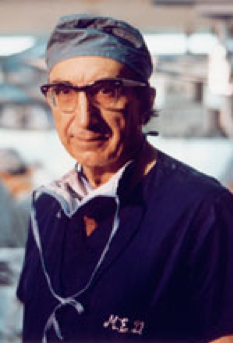
Dr. Michael E. Debakey and Dr. Williams performing an aortic reconstruction at Ben Taub Hospital, Houston, Texas in 1997.
more about dr. williams
A family of Physicians

Dr. Michael E. Debakey
Dr. Debakey’s training program at Baylor College of Medicine in Houston, Texas is legendary for requiring residents to work long hours and perform more surgeries than any other in the United States. Surgical “residents” are called this because they spend so many hours a day training to become a surgeon that they effectively reside at the large hospitals they serve. Surgical residency programs are prestigious and coveted positions for new medical school graduates. It takes at least 5 years of surgery residency training to be able to practice surgery independently. At Baylor, anything less than perfection was unacceptable from Dr. Debakey’s surgical residents
I still wanted to be a neurologist until I realized that surgery fascinated me more than the brain. My need to diagnose a problem and be capable of fixing it was insatiable. I interviewed all over the country for a surgical residency position. My travels ultimately led to Houston, where my father had trained at Baylor College of Medicine.
Baylor is legendary for its intense demeanor and quality surgical training. Dr. DeBakey loomed large over everything at the entire institution.
At the large Houston trauma hospital, Ben Taub General Hospital, surgical residents had great autonomy. We would decide which trauma patient, and in what order, we would operate upon through the day and night. It was similar to the triage process of the M*A*S*H* units that Dr. DeBakey developed for the military during World War II and the Korean War with the Army Office of the Surgeon General. Many residency programs do not give their young surgeons the level of responsibility that we had at Baylor. Our training motto was “See one, do one, teach one.” We all developed great confidence and skill from this training process.

Dr. Michael E. Debakey and myself performing an aortic reconstruction at Ben Taub General Hospital, Houston, TX, 1997.
A large part of my training was working with the experts in cancer treatment at the M. D. Anderson Cancer Center (MDACC). Also located in the Texas Medical Center, MDACC is the largest and most prestigious dedicated cancer hospital in the United States. My general surgery rotations there exposed me to the team approach to breast cancer. This multidisciplinary team concept is what I created at the UVA Community Health Breast Center in Haymarket, Virginia.
In 1999, I began surgical practice in Northern Virginia. I initially practiced general surgery, but ultimately specialized in breast surgery over a 15 year period. I then established the UVA Community Health Breast Center in 2009. In November 2018, I began an exclusive practice of breast surgery in partnership with Galaria Plastic Surgery & Dermatology.
Professionally, I am most proud to have applied to breast cancer care the same pursuit of excellence that I learned from Dr. DeBakey and his associates at Baylor. Each day, I try to apply a singular focus on every patient as a unique individual. To me, these lifelong relationships are the most rewarding aspect of being a physician and why I enjoy every day going to work.
I tend to accomplish personal goals in 5-year phases. After shifting my general surgical practice to only breast cancer in 2005, I then created the UVA Community Health Breast Center in 2010, then founded the Breast Cancer School for Patients in 2018, and was appointed Chair of the President’s Cancer Panel in 2019. All of these efforts to help others is predicated on the daily support I have from my family, friends and healthcare partners.
In 2018, I launched the very first video-based educational website for breast cancer patients. The Breast Cancer School for Patients is a national, not for profit patient educational online platform. This video-based website is a leap forward in communicating the complex concepts of breast cancer care to women who are newly diagnosed. It is a vast improvement on the exisiting “information only” websites available online. The Breast Cancer School for Patients is a separate entity from my clinical practice or my associates practice or business entity.
Over the years, family and friends have called me for advice about their breast care. After a quick conversation, they were incredibly empowered to ask their own doctors exactly what was needed. You simply get better care when you know about the important topics and the questions to ask. Currently, the medical profession does not actually “teach” patients how to obtain quality, cutting-edge care in their communities. This is a missing link in our collective efforts to provide better quality breast cancer care in the United States. This is why we created the website, to fill this online information gap.
I feel it should be our duty in healthcare to teach you what you need to know before you consult with your breast cancer physicians. This way you can be more engaged with your physicians about the complexities of cancer care. This information must be readily available online, well organized, and in short video format. Our sole mission at the Breast Cancer School for Patients is to fill this patient information gap online. You will make better treatment decisions when you are taught to be an “expert” in your own breast cancer care and will help you make better decisions with the breast specialists in your own community.